Biliopancreatic Diversion with Duodenal Switch (BPD-DS) Weight-Loss Surgery
What is BPD/DS weight-loss surgery?
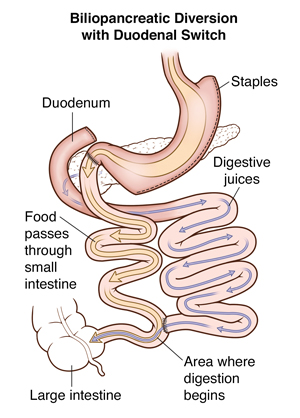
Biliopancreatic diversion with duodenal switch (BPD/DS) is a type of surgery to cause weight loss. It's also known as the duodenal switch. This type of bariatric surgery changes the size of your stomach and the length of your small intestine. It limits how much food you can eat, digest, and absorb. BPD/DS is not done as much as other weight loss surgeries.
Part of the stomach is closed off with staples to create a smaller pouch. The rest of the stomach is removed. This small stomach restricts the amount of food you can eat at one time. The small intestine (first part or duodenum) is then divided. A very short length of the last part of the small intestine is brought up and attached to it (duodenum). This is the duodenal switch. When you eat, the food then only goes through the new stomach pouch. It empties into the last part of the small intestine. This goes around (bypasses) a large section of the small intestine, so that less of the food is digested. You absorb fewer calories and nutrients. This can cause a lot of weight loss. The part of the small intestine that has been separated is reconnected to the last part of the small intestine. This changes the normal way that bile and digestive juices break down food. This is the biliopancreatic diversion. This cuts back on how many calories you absorb, causing still more weight loss.
This surgery can lead to nutritional problems over time and other complications. Talk with your healthcare provider about the risks and benefits of this surgery for you.
Why might I need BPD/DS weight-loss surgery?
This surgery can help reduce obesity and related illnesses. These include heart disease, high blood pressure, and type 2 diabetes. BPD/DS can cause a lot of weight loss. It can cause more weight loss than a gastric bypass or a sleeve gastrectomy.
Healthcare providers may advise BPD/DS to people who are obese. This means a body mass index (BMI) of 35 or greater. They may also advise the surgery for a BMI of 30 or more, with serious type 2 diabetes and other health problems, such as:
-
High blood pressure
-
High cholesterol
-
Heart disease
-
Sleep apnea
-
Lung disease
-
Nonalcoholic fatty liver disease
-
Asthma or some other breathing problems
-
Not qualifying for other surgeries due to obesity
-
Inability to achieve substantial or sustainable weight loss, or improvement in related illnesses, with nonsurgical weight-loss methods
What are the risks of BPD/DS weight-loss surgery?
All surgeries have some risks. The risks of BPD/DS include:
-
Infection, such as pneumonia, intra-abdominal abscesses, or C. diff colitis, which can lead to septic shock. (Septic shock is a life-threatening condition in which an infection spreads throughout the body and affects the internal organs.)
-
Leaks or blockage where tissue is sewn or stapled together (anastomosis)
-
Need for more surgery to fix problems
-
Acid reflux (heartburn) and esophagitis. This is irritation of the esophagus, the tube from your mouth to your stomach.
-
Dumping syndrome that causes diarrhea and cramping when food moves too fast through the stomach
-
Kidney failure
-
Depressed mood or other emotional issues
-
Blood clots in the legs that may travel to the lungs (pulmonary embolism)
-
Injury to the spleen that may lead to removal of the spleen
-
Ongoing vomiting
-
Hernia at an incision site or inside the abdomen
-
Complications from anesthesia
-
Blockages in the intestines, known as bowel obstruction
-
Bleeding, which may need transfusions
-
Heart Attack
-
Rhythm problems with the heart
-
Stroke
-
Death
BPD/DS makes it hard for the body to absorb vitamins and minerals. People who have BPD/DS may have:
-
Not enough protein (protein malnutrition)
-
Low levels of calcium and iron
-
Low levels of fat-soluble vitamins such as A, D, E, and K
-
Low level of thiamine. This is rare but can damage the nervous system.
These can lead to serious, long-term problems, such as:
-
Not enough red blood cells (anemia)
-
Thinning bones (osteoporosis)
-
Kidney stones
-
Severe life-threatening protein malnutrition called kwashiorkor (rare)
You will need to take vitamin and mineral supplements for life. You will also need to have blood tests regularly. This is to prevent severe malnutrition and related problems. Even if you take supplements, you still may have nutrition problems and need treatment.
You may also have problems, such as:
-
Dehydration if you don’t drink enough fluids
-
Gallstones
-
Short-term (temporary) hair loss
-
Stomach cramping and diarrhea after eating fat
-
Failure to meet your weight loss goals
-
Weight regain
-
Loose folds of skin that may need surgery to remove
Bariatric surgery will change your eating habits for the rest of your life. Make sure you fully understand the risks and benefits for you. Your own risks and benefits may vary according to your age and your general health. Talk with your healthcare provider to find out what risks may apply to you.
How do I get ready for BPD/DS weight-loss surgery?
You will need to go through an in-depth process to be approved for bariatric surgery. This is done to find out if you are ready for the surgery, and if it will help you. And you will need to find out if your health insurance plan will cover the costs of the surgery. You’ll need to meet with healthcare providers, such as a surgeon, a special bariatric nurse, and a dietitian with experience in BPD/DS.
Talk with your healthcare team how to prepare for your surgery. Tell your healthcare provider about all the medicines you take. This includes over-the-counter medicines, vitamins, herbs, and other supplements. You may need to stop taking some medicines before the procedure, such as blood thinners and aspirin.
You will need some tests before the surgery, such as:
-
Blood tests, to check your overall health
-
Chest X-ray to check your lungs
-
Electrocardiogram (ECG) to check your heart rhythm
You will generally also be told to:
-
Stop smoking.
-
Lose weight by following a special diet.
-
Get counseling to discuss emotional health and disordered eating habits.
-
Read educational material that will be given to you or attend classes about the procedure, expected results, and possible complications.
Tell your healthcare provider if you:
-
Have had any recent changes in your health, such as an infection or fever
-
Are sensitive or allergic to any medicines, latex, tape, or anesthetic medicines (local and general)
-
Have a history of bleeding disorders
-
Are taking any blood-thinning (anticoagulant) medicines, including aspirin, ibuprofen, or other medicines that affect blood clotting
-
Are pregnant or think you may be pregnant
-
Use a CPAP or BiPAP machine for sleep apnea or another breathing disorder
Also:
-
Ask a family member or friend to take you home from the hospital. You can’t drive yourself.
-
Follow any directions you are given for not eating or drinking before surgery.
-
Follow all other instructions from your healthcare provider.
-
Ask which medicines you should stop taking before surgery and for how long, and which medicines should be taken the day of surgery.
-
Bring your CPAP or BiPAP machine to the hospital on the day of your surgery.
You will be asked to sign a consent form that gives your healthcare provider permission to do the procedure. Read the form carefully. Ask questions if something is not clear.
What happens during BPD/DS weight-loss surgery?
BPD/DS can be done as laparoscopic surgery. This is done with several small cuts (incisions). Tiny tools and a small tube with a light and tiny camera are put into the small incisions. Some surgeons use robotic tools to help do part of the surgery.
In some cases, BPD/DS may be done as open surgery. For this method, the surgeon makes one larger incision instead of several smaller ones. They see and use tools through this incision.
The surgery generally follows this process:
-
You will be given anesthesia to block pain and make you sleep through the surgery.
-
The surgeon will make incisions.
-
The surgeon will close off part of the stomach with staples to create a smaller new stomach pouch. The rest of the stomach is removed through an incision.
-
The first part of the small intestine (called the duodenum) is divided. A very short length of the last part of the small intestine is brought up and attached to it.
-
The bypassed part of the small intestine is reconnected to the last part of the small intestine.
-
The surgeon will then remove the tools and close the incisions with stitches (sutures), staples, or surgical glue.
What happens after BPD/DS weight-loss surgery?
You will wake up in a recovery room. You will be given medicine to control pain. You will be moved to a hospital room. You will be asked to get out of bed to move around within the next day. This helps prevent blood clots in your legs. You will have liquid nutrition. Your team will tell you when you're ready to go home.
At first, you may have stomach or bowel cramping, or nausea. Tell your healthcare provider if pain or nausea is severe or doesn’t improve with time. Take pain medicines as prescribed. Your healthcare team will tell you when it’s OK to shower, drive, return to work, exercise, and lift objects.
Call your healthcare provider if you have any of the following:
You will get instructions about how to adapt to your new diet after your surgery. You will likely be on liquid nutrition for a few weeks after surgery. Over time, you’ll start to eat soft foods and then solid foods. If you eat too much or too fast, you will likely have stomach pain or vomiting. You’ll learn how to know when your new stomach is full.
Your healthcare provider or nutritionist will give you more instructions about your diet. You’ll need to learn good habits like choosing healthy foods and not skipping meals. Your healthcare provider or nutritionist will also need to screen you for low levels of nutrients.
You will need to take daily supplements after BPD/DS surgery. These include:
Work with your healthcare team after surgery to stay healthy. Make sure to:
-
Follow the nutrition plan set up by your dietitian.
-
Get regular physical activity. Start slowly and build up to more activity.
-
Talk with a counselor or weight-loss surgery support group to help you adjust.
When to call your healthcare provider
Call your healthcare provider if any of the following occur:
-
A fever of 100.4°F (38°C) or higher , or as directed by your healthcare provider
-
A red, bleeding, or draining incision
-
Frequent or persistent nausea or vomiting
-
Increased pain at an incision
-
Pain or swelling in your legs
Call 911
Call 911, or get immediate medical care at the nearest emergency room if any of the following occur:
Next steps
Before you agree to the test or procedure make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure