Discharge Instructions: Biliary Catheter
You are going home with a biliary catheter in your body. This is a small, flexible tube placed into the common bile duct. It's used when this duct becomes blocked. The catheter allows a fluid (bile) to flow from the gallbladder and liver to the small intestine. The catheter can drain the bile inside your body. Or it can drain the bile into a bag outside your body. Your health care provider talked with you about how long the biliary catheter will need to be in place. This sheet gives you general guidelines on caring for your catheter.
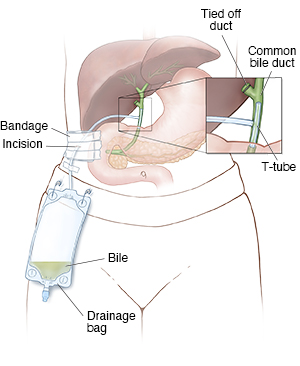 |
| Outside catheter. |
General guidelines
If you have an outside catheter:
-
Empty your catheter bag before it is completely full.
-
Don’t go swimming, take baths, or soak in a hot tub.
-
Shower as needed, but keep the tube and the area around it dry. Ask your provider about the best way to do this. You may cover the area with waterproof material, such as plastic wrap. Tape the edges of the plastic wrap to your skin so that water cannot get under it. If the area does get wet, dry your skin completely.
-
Change your dressing (split gauze sponges, gauze, and tape) every 3 days, or as advised by your provider. Change it more often if it becomes wet, dirty, or loose.
-
Avoid activities that cause a pulling sensation or pain around the catheter.
-
Follow your provider's instructions about diet, including which foods to avoid.
Changing the dressing
Change your dressing (split gauze sponges, gauze, and tape) every 3 days, or as advised by your provider. Change it more often if it becomes wet, dirty, or loose. Below are general guidelines for cleaning around the catheter and changing the dressing.
1. Gather your supplies
Gather these items:
-
Clean washcloths and towels.
-
Mild soap and warm water.
-
Nonstick gauze pads.
-
Clear, waterproof bandages.
-
Scissors.
-
Split gauze sponges.
-
Gauze pads (4-inch square).
-
Tape.
-
A connecting tube and a clean drainage bag, if needed.
-
A plastic bag to dispose of supplies.
2. Remove the old dressing
-
Wash your hands well using mild soap and clean, running water. Be sure to clean between your fingers and under your nails.
-
Remove the old dressing. Be careful not to pull on the drainage catheter. Keep the plastic ring against the skin.
-
Check the skin around the catheter. Look for any redness, soreness, or fluid. Ask your provider about applying an antibiotic cream.
-
Gently wash the area around the catheter with a soapy washcloth. Pat it dry with a clean towel.
-
Do not use creams, powders, lotions, oils, or sprays near this area.
-
Wash your hands well again. Use soap and clean, running water.
3. Apply the new dressing
-
Cut a round piece of nonstick gauze pad, slightly larger than the plastic ring. Cut a slit in the nonstick gauze pad so that it will fit around the catheter. Place the nonstick gauze pad under the blue disk.
-
Fold a new clear, waterproof bandage in half. Cut a hole in the center. The hole should be about the size of the nipple on the plastic ring. Put the catheter through this hole. Apply the clear, waterproof bandage to your skin. If the catheter is attached to a drainage bag, you must first disconnect the bag. Then slip the catheter through the clear, waterproof bandage.
-
Place 2 split gauze sponges around the catheter.
-
Fold a 4-by-4-inch gauze pad on each side of the catheter. You should be able to curl the catheter once without twisting (kinking) it. The catheter should rest on the gauze and not on your skin.
-
Cover the catheter with a 4-by-4-inch gauze pad. Use tape to hold the dressing in place. Check for kinks in the tube, and move the tube around if it is not draining.
-
Put a piece of tape below the dressing to hold the catheter. This will also act as a safety device.
-
Clean the external drainage bag by rinsing it out with soap and water. Allow it to air-dry well. Have 2 drainage bags on hand so that you can wear one while cleaning the other. Always keep one bag clean and ready for use.
Flushing the catheter
-
Always wash your hands well before working with your catheter.
-
Open the cap and wipe it clean with alcohol. Attach a syringe that is prefilled with normal saline. Do this by turning it clockwise until it's in the locked position. (Your provider will tell you what size syringes and how much normal saline to use.)
-
Using the plunger, slowly push down.
-
The saline should infuse easily. If you meet resistance, stop and call your home health care provider.
Follow-up care
-
Follow up with your health care provider, as advised.
-
Keep all follow-up appointments. Your provider will need to check your tube once a month. Your provider will change it every 8 to 12 weeks.
When to call your health care provider
Call your health care provider if you have any of these:
-
A plastic ring that comes away from the skin.
-
A catheter that gets twisted and can’t be straightened.
-
A catheter that stops draining into the bag.
-
A catheter that is blocked or has bile leaking around the catheter site.
-
A catheter that falls out.
-
Grit or stones in the catheter.
-
A skin rash.
-
Signs of infection, such as redness, soreness, or blood or pus leaking around the catheter site.
-
Sudden pain.
-
A fever of 100.4°F (38°C) or higher, or as advised by your provider.
-
Chills.
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Sabrina Felson MD
Online Medical Reviewer:
Vinita Wadhawan Researcher
Date Last Reviewed:
10/1/2024
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.