When Your Child Has Non-Hodgkin Lymphoma
Your child has been diagnosed with non-Hodgkin lymphoma (NHL). You're likely feeling shocked and scared. You're not alone. Support and treatment are available. Your child’s healthcare team will help you as you make important decisions about your child’s health.
What is NHL?
NHL is cancer that starts in cells in the lymphatic system. The lymphatic system is part of the immune system, which helps the body fight infection. The lymphatic system includes:
-
Lymph. A clear, infection-fighting fluid that carries a type of white blood cell called lymphocytes. Lymph flows through lymph vessels. These are a system of thin tubes that go all over the whole body, much like blood vessels. Lymph enters the blood in a vein near the heart.
-
Lymph nodes. Small, bean-shaped organs that filter lymph and store white blood cells. Lymph nodes are grouped together all over the body. Some places where they are found include the neck, armpit, and groin. Sometimes lymph nodes swell when you have a cold or infection. In rare cases, they swell when cancer is growing in the lymph node.
-
Bone marrow. Soft, spongy tissue found in the center of bones. Blood cells are made in the bone marrow.
-
Thymus. A gland that helps build the immune system in young children. It makes a type of white blood cell called T-lymphocytes, which fight infection. The thymus is behind the breastbone in the chest.
-
Spleen. Organ that makes and stores lymphocytes and filters the blood. It’s near the stomach under the ribs on the left side of the body.
-
Other organs. Lymphatic tissue is also found in other organs, such as the tonsils, thyroid gland, skin, and digestive tract.
With NHL, lymphocytes change (mutate) and grow out of control in the lymphatic system. When the mutated lymphocytes (lymphoma cells) collect in a lymph node or organ, such as the spleen, they form a tumor. The cancer cells can spread (metastasize) to another part of the lymphatic system, like the bone marrow or spleen. They can also spread outside the lymph nodes to almost any part of the body. The lymphoma cells crowd out healthy blood cells and make it hard for the body to fight infection. They can also cause other health problems.
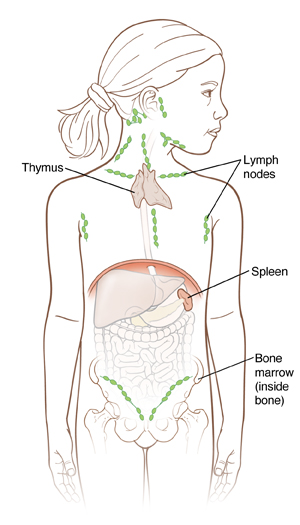 |
| Lymph nodes, bone marrow, the spleen, and the thymus gland are all parts of the lymphatic system. This system works to help the body fight infection. |
Who gets NHL?
Children can get NHL at any age. But kids between ages 10 and 19 are affected most often. NHL is uncommon in children younger than age 5. NHL affects boys more often than girls. NHL isn't contagious. This means your child can’t pass it to another person.
What causes NHL?
With NHL, white blood cells called lymphocytes start to grow out of control. If the abnormal cells come together in lymph nodes or other parts of the body, they can form tumors. Doctors don't fully know what causes this. Changes in certain genes (mutations) may affect the way your child’s cells grow. This gene mutation is often random and couldn’t have been prevented.
Having a weak immune system or certain rare inherited diseases can increase your child's risk for NHL. In rare cases, other factors may play a role. This includes being exposed to certain viruses, chemicals, medicines, or radiation. But most often, the cause of cancer in children is unknown.
What are the symptoms of NHL?
Some common symptoms of NHL include fever, night sweats, and swollen lymph nodes in the neck, chest, armpits, or groin. NHL can also make your child feel very tired all the time, lose weight, and have frequent infections.
Other symptoms can depend on where the lymphoma is:
-
If the lymphoma starts in the belly (abdomen), it can cause belly pain, fever, constipation, upset stomach (nausea), vomiting, feeling full after a small amount of food, and loss of appetite. This is because the tumor is pressing on the organs in this area. The belly may look swollen and may hurt. Fluid may build up in the belly.
-
If the lymphoma starts in the chest, the child might have trouble breathing, pain with deep breaths, coughing, or wheezing. Lymphomas in the chest can also press on a main blood vessel called the superior vena cava. This can cause swelling and a bluish color in the head, neck, upper chest, and arms. If left unchecked, it can also affect the brain and may even be life-threatening.
-
If the lymphoma spreads around the brain or spinal cord, the child might have a headache, changes in vision, trouble talking, numbness on the face, and nausea or vomiting.
-
Some lymphomas can be in the skin. They can cause red or purple lumps and itchy skin.
Your child may have had some of these symptoms, or other symptoms.
What tests are done once NHL is diagnosed?
Your child has had a biopsy to diagnose NHL. This means a tiny piece of tissue (called a sample) was taken out for testing. One or more of these tests may be needed to learn more about the lymphoma:
-
Blood tests. These are done to get an idea of your child's overall health and how well their organs are working. Changes in the amount of certain substances in the blood can also be signs of disease.
-
Imaging tests. These take detailed images of the inside of the body. These tests may include a chest X-ray, MRI, CT scan, ultrasound, and PET scan.
-
Bone marrow aspirations and biopsies. Bone marrow samples are taken from the hip bones to look for lymphoma cells there.
-
Lumbar puncture (spinal tap). This takes a sample of the fluid around the spinal cord from the child’s low back. This is done to see if the lymphoma has spread to the brain and spinal cord.
What are the stages of NHL?
The stage of a cancer is how much cancer there is and how far it has spread in your body. Your child's healthcare provider uses exams and tests to find out the size of the cancer and where it is. Scans can also show if the cancer has grown into nearby areas. And if it has spread to other parts of your child's body. The stage is one of the most important things to know when deciding how to treat the cancer.
The staging process used for NHL looks at:
-
Where the main (primary) tumor is
-
If the cancer is all above or below the diaphragm. This is the breathing muscle that separates the chest from the belly.
-
If the cancer has spread to other parts of the body
The International Pediatric Non-Hodgkin Lymphoma Staging System (IPNHLSS) is a modified version of the older St. Jude staging system and is most often used for NHL in children. (A different system is used for NHL in adults.) In this system, the cancer is grouped into four stages. The stage is written as a Roman numeral and can have a value of I, II, III, or IV (1 to 4). The higher the number, the more advanced the cancer is. For instance, stage I is NHL that's in only one place and not in the chest or belly. Stage IV means the cancer is in the brain or spinal cord and/or in the bone marrow when NHL is first found.
Stages I and II are limited-stage disease and treated alike. Stages III and IV are advanced-stage disease and also treated the same way.
There are many different types of childhood NHL. Your child’s healthcare provider will talk with you about the type your child has and the stage. Ask the healthcare provider to explain the details of the cancer to you in a way you can understand. Ask any questions and talk about your concerns.
How is NHL treated?
The treatment that's best for your child depends on the type of NHL they have, where it is, and its stage. Many times, more than one kind of treatment is used. Your child may need one or more of these treatments:
-
Surgery. This isn't often done to treat childhood NHL. It may be used to get a biopsy sample, put in an infusion line (catheter), or ease symptoms caused by a tumor, such as blocked intestines.
-
Chemotherapy (chemo)orother medicines. Many different medicines and combinations of medicines can be used to kill lymphoma cells. They're given through a small tube (catheter) that’s usually put into a vein in the arm or chest. Or they may be given by mouth (oral) or as a shot (injection).
-
Radiation therapy. This treatment uses strong X-rays to help destroy lymphoma cells and shrink a tumor. It's not often used. But it may be used to shrink a tumor that's causing problems. For instance, a tumor may be pressing on nerves and causing pain. Or it may be pressing on the airways and lungs and making it hard to breathe.
-
High-dose chemo with a stem cell transplant. Young blood cells, called stem cells, are taken from the child or from someone else (a donor). This is followed by high-dose chemo and maybe radiation. This damages the bone marrow to keep it from making lymphoma cells. After the high-dose chemo, stem cells are put back in your child's body to rebuild healthy bone marrow.
Most children with NHL are treated as part of a clinical trial. Taking part in a clinical trial means your child gets the best treatment available today. They might also get new treatments that are thought to be even better. Before starting treatment, talk with your child's healthcare provider to find out if there are any clinical trials you should think about.
Supportive treatments
Supportive treatments help to protect your child from infection, ease discomfort, and keep the body’s blood counts in a healthy range. During your child’s treatment, they may be given antibiotics. These help prevent and fight infection. Other medicines may also be given to help ease side effects, such as nausea, pain, or diarrhea. Your child may also need blood or platelet transfusions to restore the blood cells destroyed by treatment.
What are the long-term concerns?
With early treatment, NHL can often be cured. But treatments like chemo and radiation may cause some problems. For instance, they can damage some organs. Your child’s health will need to be watched closely for life. This may include clinic visits, blood tests, and imaging tests. Talk with your child's healthcare provider about long-term issues linked to your child's treatment options, such as fertility issues and the risk of developing another cancer. This helps you know what to expect so you can make the best decision for your child.
Coping
Receiving a cancer diagnosis for your child is scary and confusing. Remember that you're not alone. Your child’s healthcare team will work with you, your family, and your child during your child’s illness and care. You may also want to get more information and support for yourself. Learning about your child's cancer and talking with others who also have a child with cancer may help you and your family cope with the changes the cancer brings. Some helpful resources include: