A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Topic IndexLibrary Index
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
Gastroparesis
Gastroparesis is a disorder that slows or stops the flow of food from your stomach into the small intestine. It's also called delayed gastric emptying. It's caused by a problem with motility. This is the movement of the muscles in the digestive tract.
For many people, gastroparesis is a lifelong health problem. But treatment can help ease symptoms and prevent complications. Read on to learn more about gastroparesis and how it can be managed.
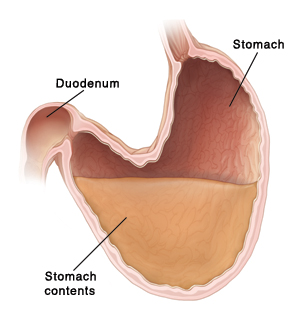 |
| Gastroparesis means that food and fluids move too slowly out of the stomach into the duodenum. |
How gastroparesis develops
With normal motility, signals from nerves tell the stomach muscles when to contract. These muscles move food from the stomach into the first part of the small intestine (the duodenum). With gastroparesis, the nerves or muscles are damaged. This causes motility to slow down or stop. As a result, food can't move from the stomach as it should into the small intestine. This delayed emptying can cause nausea, vomiting, and other symptoms. Malnutrition can result. Bezoars (hardened lumps of food) can form in the stomach and cause other problems as well.
Causes of gastroparesis
Gastroparesis can be caused by any of these:
-
Diabetes
-
Surgery of any of the digestive organs, such as the stomach and intestines
-
Certain medicines, such as strong pain medicines (opioids) and some antidepressants
-
Underactive thyroid (hypothyroidism)
-
Central nervous system disorders, such as Parkinson disease and multiple sclerosis
-
Some autoimmune diseases, such as systemic scleroderma.
-
Viral stomach infection
In many cases, the cause of gastroparesis may not be known.
Symptoms of gastroparesis
These can include:
-
Upset stomach (nausea) and vomiting
-
Feeling full quickly when eating
-
Belly pain
-
Heartburn
-
Belly bloating
-
Weight loss
-
Loss of appetite
-
High and low blood sugar levels (in people with diabetes)
Diagnosing gastroparesis
Your healthcare provider will ask about your symptoms and health history. You’ll also be examined. In addition, blood tests and X-rays are often done to check your health and rule out other problems. To confirm the problem, you may need other tests as well, such as:
-
Upper endoscopy. This is done to see inside the stomach and duodenum. For the test, an endoscope is used. This is a thin, flexible tube with a tiny camera on the end. It’s inserted through the mouth and down into the stomach and duodenum.
-
Upper gastrointestinal (GI) series. This is done to take X-rays of the upper GI tract from the mouth to the small intestine. For the test, a substance called barium is swallowed. The barium coats the upper GI tract so that it will show up clearly on X-rays.
-
Radioisotope gastric-emptying scan. This is done to measure how quickly food leaves the stomach. For the test, a meal containing a harmless radioactive substance (tracer) is eaten. Then scans of the stomach are done. The tracer shows up clearly on the scans. It shows the movement of the food through the stomach.
-
Gastric (antroduodenal) manometry. This test gives pressure measurements of the stomach and small intestine. It checks how the contractions are working.
-
Wireless capsule study. For this test, you swallow a wireless capsule. The capsule measures how well your stomach empties and how fast food and fluids move through your intestines. You'll pass the capsule out of your body with a bowel movement.
-
Gastric emptying breath test. This test checks stomach emptying. It measures how much carbon dioxide you breathe out over several hours after eating food.
-
Scintigraphic gastric accommodation. This test measures your stomach contents before and after a meal. It also checks how well your stomach relaxes after you eat food.
Treating gastroparesis
The goal of treatment is to help you manage your condition. Treatment may include 1 or more of these:
-
Diet changes. You may need to make changes to your eating habits and daily diet. For instance, your healthcare provider may tell you to eat small meals during the day. Doing this can keep you from feeling full too quickly. You may be placed on a liquid or soft diet. This means you’ll eat liquid foods or foods that are mashed or put through a blender. Plus, you may need to stay away from foods high in fats and fiber. These can slow digestion. For more help with your diet, your healthcare provider can refer you to a dietitian. In severe cases, you may need a feeding tube. This sends liquid food or medicine directly to your small intestine, bypassing the stomach.
-
Treating diabetes. If you have diabetes, it's important to control your blood sugar. High sugar levels may make gastroparesis worse.
-
Medicines. These can help manage symptoms, such as nausea and vomiting. They can also improve motility. Each medicine has certain risks and side effects. Your provider can tell you more about any medicine that's prescribed for you. Also, if you're on opioid pain relievers and certain other medicines, your provider may also advise stopping these if they're adding to your gastroparesis.
-
Surgery. You may need to have a tube surgically put into your stomach. The tube removes excess air and fluid. This can ease severe symptoms of nausea and vomiting. In rare cases, other surgery may be needed on the stomach or small intestine. This is to make a new passageway for food to be emptied from the stomach.
-
Gastric electrical stimulation. This treatment is done less often and may not be available. Your healthcare provider can tell you more about this treatment if it's a choice for you.
Diabetes and gastroparesis
If you have diabetes, gastroparesis can make it harder to manage your blood sugar level. You’ll need to take extra steps in your treatment to prevent complications. Work with your healthcare provider to learn what you can do to protect your health. For more information, contact the American Diabetes Association.
Long-term concerns
With treatment, most people can manage their symptoms and keep up their normal routines. If your symptoms are moderate to severe, you may need to see your healthcare provider more often for checkups. If you have a long-term (chronic) health problem that may be linked to gastroparesis, such as diabetes, regular follow-ups are vital. These can help keep track of your blood sugar control. This is key to successfully managing both conditions. Also, other treatments will likely be needed.
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Robyn Zercher FNP
Date Last Reviewed:
3/1/2024
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.