Biliary Atresia in Children
What is biliary atresia in children?
Biliary atresia is a rare liver disease that occurs in newborn babies. It's often found shortly after birth. The disorder affects tubes in the liver called bile ducts. If not treated with surgery, it can be fatal.
Bile is a fluid made by the liver. Normally the bile ducts take bile to the small intestine. Bile helps with digestion and also carries waste products. When a child has biliary atresia, the bile ducts in the liver are blocked. Bile becomes backed up in the liver. This damages the liver. Many vital body functions also are affected.
There are 2 types of biliary atresia:
-
Perinatal biliary atresia. This is the most common type. It appears after birth, most often when a baby is about 2 weeks to 8 weeks old.
-
Fetal biliary atresia. This is less common. It appears while a baby is still developing in the mother’s womb.
Biliary atresia must be treated with surgery. It's the most common cause of liver transplants in children in the U.S. It's more common in girls than in boys.
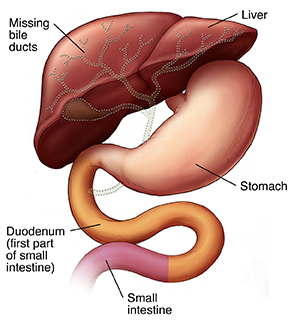 |
| The dotted lines show areas that can be affected by biliary atresia. |
What causes biliary atresia in a child?
Experts don’t know what causes biliary atresia. It's not passed down from parent to child, so it's not an inherited disease.
Researchers are looking at possible causes, such as:
Which children are at risk for biliary atresia?
Premature babies are at greater risk for biliary atresia than full-term infants.
What are the symptoms of biliary atresia in a child?
Babies with biliary atresia usually seem healthy at birth. Most often, symptoms start between 2 weeks to 8 weeks of life. Symptoms may include:
-
Yellowish skin and eyes (jaundice).
-
Dark urine (yellow-stained diapers).
-
Pale, almost white stools.
-
Swollen belly (abdomen).
-
Weight loss.
Symptoms of biliary atresia may look like other liver conditions or health problems. Always see your child's doctor for a diagnosis.
How is biliary atresia diagnosed in a child?
Your child’s doctor will give your child an exam and take a health history. The doctor may also do several tests. These may include the following.
Blood tests
-
Liver enzymes. High levels of liver enzymes can alert doctors to liver damage or injury. That’s because the enzymes leak from the liver into the bloodstream when the liver is damaged.
-
Bilirubin. Bilirubin is made by the liver and is sent out into bile. High levels of bilirubin often mean that bile flow is blocked. Or it could mean there is a defect in the processing of bile by the liver.
-
Albumin and total protein. Below-normal levels of proteins made by the liver are linked to many long-term (chronic) liver disorders.
-
Clotting studies. These include PT (prothrombin time) and PTT (partial thromboplastin time). These tests check how long it takes for blood to clot. Blood clotting requires vitamin K and proteins made by the liver. Liver cell damage and blocked bile flow can both cause problems with normal blood clotting.
-
Viral studies, including hepatitis and HIV. These check for viruses in the bloodstream.
-
Blood culture. This checks for bacterial infection in the bloodstream that can affect the liver.
Imaging tests
-
Abdominal ultrasound. This is a diagnostic imaging test that uses high-frequency sound waves and a computer to make images of blood vessels, tissues, and organs. Ultrasounds are used to see the liver, gallbladder, and bile ducts.
-
HIDA or hepatobiliary scan. A low-level radioactive isotope is injected into your child's vein. The liver and intestine are scanned by a nuclear medicine machine. If the isotope passes through the liver into the intestine, the bile ducts are open and the child does not have biliary atresia.
Other tests
-
Liver biopsy. A tissue sample is taken from your child's liver and checked for any problems. A biopsy can tell if biliary atresia is likely. It may also rule out other liver problems.
-
Diagnostic surgery (such as intraoperative cholangiogram). The surgeon can see the liver and bile ducts by making a cut or incision in your child’s belly or abdomen. If biliary atresia is diagnosed, the surgeon may treat it with surgery at the same time.
-
Endoscopic retrograde cholangiopancreatography (ERCP). During this procedure, a lighted tube is placed down the mouth into the small intestine to get a better idea of the cause of biliary disease.
How is biliary atresia treated in a child?
Without surgery, biliary atresia can be fatal. Two types of surgery are used to treat this condition. Your child's doctor will discuss which surgery would be a good choice for your child.
Kasai procedure
This surgery connects the bile drainage from the liver directly to the intestinal tract. It goes around (bypasses) the blocked bile ducts. This surgery can allow a child to grow and be in fairly good health for a few years to adulthood. At some point, bile may back up into the liver and cause liver damage. Your child may also need a liver transplant over time if the liver damage already done is severe enough and eventually causes the liver to fail. Undergoing the Kasai procedure as a newborn will allow your child to grow enough and postpone the need for a liver transplant until your child is older.
Your child will need good nutrition, as well as vitamin supplements and medicines as instructed by their doctor. Medicines may include postoperative steroids and a choleretic (such as ursodeoxycholic acid) to increase bile flow.
Liver transplant
A liver transplant removes the damaged liver and replaces it with a new liver from a donor. The new liver may be:
-
A whole liver, received from a donor who has died.
-
Part of a liver, received from a donor who has died.
-
Part of a liver, received from a relative or other person whose tissue type matches the child's tissue type.
After a liver transplant, the new liver begins working and the child's health often gets better quickly.
After a transplant, a child must take medicines to help prevent the body’s immune system from attacking, or rejecting, the new liver. These medicines are called antirejection medicines. Rejection is part of the immune system’s normal way of fighting against viruses, tumors, and other foreign substances. Antirejection medicines weaken the immune system’s response.
It’s important to have regular contact with your child’s doctor and members of the transplant team after a liver transplant.
What are possible complications of biliary atresia in a child?
Biliary atresia causes liver damage and affects many processes that allow the body to work normally. Without surgery, the disease can be fatal.
Even after surgery, babies with biliary atresia are at risk for cholangitis, an infection of the bile ducts that can spread to the liver. This needs immediate treatment with IV (intravenous) antibiotics.
Malnutrition and failure to thrive are common in children with biliary atresia.
How can you help your child live with biliary atresia?
Before your child has surgery, nutrition may be a problem. With biliary atresia, not enough bile reaches the intestine to help digest fats in the diet. Liver damage can cause a lack of protein and a lack of vitamins. Children with liver disease need more calories than a normal child because they have a faster metabolism.
Your child’s doctor may recommend that your child see a pediatric nutritionist. The nutritionist can advise you on your child's diet. A nutritional plan may include a balanced diet and added vitamins, as directed by your child’s doctor.
Some children with liver disease become too sick to eat normally. If this is the case, your child’s doctor may also recommend that you give high-calorie liquid feedings. These feedings are given through a tube called an NG (nasogastric) tube. The tube is guided into your child’s nose, down the esophagus, and into the stomach. A high-calorie liquid can be given through the tube to add to your child's diet if your child can eat only small amounts of food. Or it can replace meals if your child is too sick to eat.
After surgery, your child's digestion may go back to normal. Or you may still need to give your child extra vitamins or adjust your child's diet. Talk with your child's doctor for recommendations.
Many factors affect how well children with biliary atresia do over time. These factors include:
-
How much damage occurred to the bile ducts.
-
At what age the child had either a Kasai procedure or liver transplant.
-
How much liver damage has occurred.
-
The child’s overall health.
After a liver transplant, your child's health will typically improve. But your child must follow a strict medical routine. This includes taking:
-
Medicines to prevent the body’s immune system from attacking, or rejecting, the new liver. These are called antirejection medicines. They weaken the immune system’s response.
-
Medicines to prevent infection, called antibiotics.
-
Other medicines may be prescribed, and some new medicines are being investigated to see if they help.
It's important to work closely with your child's doctors.
When should you contact your child's doctor?
Contact your child’s doctor right away if you see that your child:
-
Has yellowish skin and eyes (jaundice).
-
Has very dark, almost brown-colored urine.
-
Has pale, almost white stools.
-
Is not gaining weight.
Also contact your child’s doctor to ask what symptoms you should look for if your child:
Key points about biliary atresia in children
-
Biliary atresia is a rare liver disorder that occurs in newborn babies.
-
Experts don’t know what causes the disease.
-
If not treated with surgery, biliary atresia can be fatal.
-
At some point, even with a diagnosis right away, surgery, and the best care, your child may need a liver transplant.
-
After a liver transplant, your child must take medicines to stop the body from attacking, or rejecting, the new liver.
Next steps
Tips to help you get the most from a visit to your child’s doctor:
-
Know the reason for the visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your doctor gives you for your child.
-
Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are and when they should be reported.
-
Ask if your child’s condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if your child does not take the medicine or have the test or procedure.
-
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your child’s doctor after office hours. This is important if your child becomes ill and you have questions or need advice.