When Your Child Needs an Upper Endoscopy
An upper endoscopy is a test that shows the inside of the upper gastrointestinal (GI) tract. This includes the esophagus, stomach, and the first part of the small intestine (duodenum). The healthcare provider can take tissue samples (biopsy), check for problems, or remove swallowed objects. The test normally takes about 15 to 20 minutes.
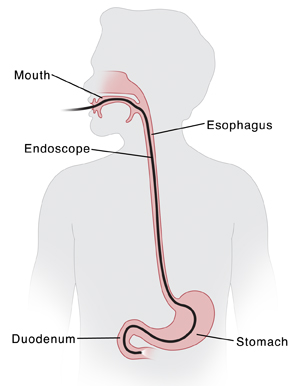 |
| An endoscope gives the doctor an inside view of the upper GI tract. |
Let the healthcare provider know
For your child’s safety, let the healthcare provider know if your child:
-
Is allergic to any medicine, sedative, or anesthesia
-
Is taking any medicine, especially aspirin
-
Has heart or lung problems
During the test
An upper endoscopy is done by a healthcare provider in an office, testing center, or hospital. During the test you can expect the following:
-
You can often stay with your child in the testing room until your child falls asleep.
-
Your child lies on an exam table.
-
Your child is given a pain reliever and a medicine that makes them relax or sleep (sedative). This is done through an IV (intravenous) line. Or your child is given medicine that makes them sleep (anesthesia) by facemask or IV. A trained nurse or anesthesiologist helps with this process and also watches your child. Special equipment is used to check your child’s heart rate, blood pressure, and blood oxygen levels.
-
Your child’s throat is numbed with a spray or gargle.
-
A bite block is placed in your child’s mouth. This prevents your child from biting down on the endoscope.
-
The endoscope is guided down your child’s throat. This is a long, flexible tube with a light and a camera at the end. It doesn’t affect your child’s breathing.
-
Air is put through the endoscope to expand your child’s stomach and upper GI tract.
-
Images of your child’s stomach and upper GI tract are viewed on a screen as the endoscope advances.
-
The healthcare provider may take tissue samples or do procedures, as needed.
After the test
-
Your child is taken to a PACU (postanesthesia care unit) to be watched as they wake up. It may take 1 to 2 hours for the medicines to wear off.
-
Unless told not to, your child can return to their normal routine and diet right away.
-
The healthcare provider may discuss early results with you after the test. You’re given complete results when they’re ready.
Helping your child get ready
You can help your child by preparing them in advance. How you do this depends on your child’s needs:
-
Explain that the healthcare provider is testing the upper GI tract. Use brief and simple terms to describe the test. Younger children have shorter attention spans, so do this shortly before the test. Older children can be given more time to understand the test in advance.
-
As best you can, describe how the test will feel. An IV is inserted into the arm to give medicines. This may cause a brief sting. Your child won’t feel anything once the medicines take effect.
-
Allow your child to ask questions.
-
Use play when helpful. This can include role-playing with a child’s favorite toy or object. It may help older children to see pictures of what happens during the test.
When to call the healthcare provider
Call your healthcare provider right away if your child:
-
Coughs up a large amount of blood right after the test (more than a spoonful)
-
Has a sore throat that doesn’t go away
-
Vomits
-
Has belly (abdominal) pain that doesn’t go away
-
Has problems swallowing
-
Has fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Has chest pain that doesn’t go away ( Call 911)
How to take a child's temperature
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Online Medical Reviewer:
Liora C Adler MD
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Tara Novick BSN MSN
Date Last Reviewed:
12/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.