Diabetes and Your Child: Low Blood Sugar
Low blood sugar (hypoglycemia) happens when there is too little sugar (glucose) in your child’s blood. It can be caused by skipping meals or snacks, eating too little food, or taking too much insulin or diabetes medicine. A lot of physical activity can also cause low blood sugar, even hours later.
How to recognize a low blood sugar level
Everyone’s symptoms are different. Your child may feel dizzy, weak, hungry, headachy, sweaty, or shaky. Your child may seem cranky or confused. They also may seem to be having nightmares or crying out in their sleep. Severe hypoglycemia can cause seizures. If lows happen very often over time, your child may no longer be able to sense them (hypoglycemia unawareness). Encourage your child to recognize their symptoms and tell you about them right away. Slightly low blood sugar levels may go unnoticed, however, in severe cases, low blood sugar can cause seizures or passing out. This requires urgent medical care.
What to do
Actions to take include:
-
Stay calm so you can better help your child.
-
Check your child’s blood sugar to make sure that it is low. If you’re not able to check, treat for low blood sugar anyway.
-
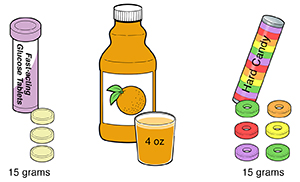
Give your child 15 to 20 grams of fast-acting sugar. Examples are 3 to 4 glucose tablets, a tube of sugar gel, some cake icing, or 4 ounces (½ cup) of juice or regular soda. Diet soda will not help at all. Chocolate, cookies, and other fatty sweets will not work fast enough.
-
Don't use carbohydrate sources high in protein such as milk or nuts. These may increase the insulin response to dietary carbohydrates.
-
If possible, recheck blood sugar in 15 minutes. If it is still low, give your child another 15 to 20 grams of fast-acting sugar.
-
Once your child’s blood sugar is normal, give your child a snack or meal to eat.
-
If your child’s blood sugar does not go back up, call your healthcare provider or take your child to the emergency room.
How to prevent low blood sugar
These tips may help your child:
-
Check that your child eats meals and snacks on time, and eats before exercising.
-
Have your child carry fast-acting sugar.
-
Don’t inject insulin near a muscle that’s going to be exercised.
-
Check your child’s blood sugar often, especially after exercise and at bedtime.
-
In an age-appropriate way, teach your child about low blood sugar and how to manage it.
-
Ask your child's healthcare provider if your child can take rapid-acting insulin that can be given after the meal. That way, you will be sure how much your child has eaten before they get their shot.
-
Keep a detailed log of your child's blood sugar levels, including any lows. Talk about these with your child's healthcare provider at the next check-up. If your child keeps having low blood sugar, ask about an insulin pump. Your child may do better with a pump instead of many injections.
Tips
Other tips include:
-
Have your child wear or carry a medical ID that states that they have diabetes and includes who to contact in case of an emergency.
-
Always keep an emergency diabetes kit close at hand. Check that your child's school or daycare also has an emergency kit.
Glucagon medicine
For severe low blood sugar levels, your child may need glucagon. Your child may also need this if they can't take oral glucose because they are vomiting, are too sluggish to swallow, or are unconscious. Glucagon is a medicine that frees the glucose already stored in your child's body. Glucagon is available as an injection or as a powder that's put into the nose. Nasal glucagon is approved for children 4 years and older. Ask your child's healthcare provider which type of glucagon is best for your child. Ask about glucagon emergency kits for home and school. Have the provider teach you when and how to use glucagon. Make sure other caregivers for your child know how to use it in case of an emergency.
Online Medical Reviewer:
Dan Brennan MD
Online Medical Reviewer:
Jessica Gotwals RN BSN MPH
Online Medical Reviewer:
Shaziya Allarakha MD
Date Last Reviewed:
3/1/2024
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.