A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Back to Intro
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
Prostate Biopsy
Cancer occurs when abnormal cells grow uncontrollably to form a tumor. Prostate cancer is the type of cancer that starts in the prostate gland. The prostate is a small, walnut-shaped organ located under the urinary bladder and in front of the rectum. It produces the fluid in the semen that nourishes and transports sperm
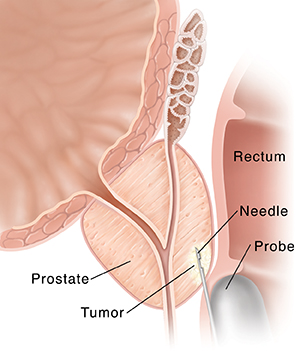
Early tests that may indicate cancer of the prostate include a digital rectal exam, a PSA (prostate specific antigen blood test), ultrasound, and others. A core needle biopsy will be done if your healthcare provider thinks you have prostate cancer. A thin needle is used to remove small samples of prostate tissue. Often a few biopsies are taken. These samples are sent to a lab to be examined under a microscope to confirm whether cancer cells are present.
Taking tissue samples
A biopsy takes about 15 to 20 minutes. You may be given an enema or suppository before the biopsy to clear the bowels. Antibiotics are given at least 1 hour before the biopsy. During the procedure:
-
You'll be given antibiotics to prevent infection.
-
You may be given a sedative, local pain killer, or pain medicine.
-
A small ultrasound probe is put into the rectum as you lie on your side. A picture of your prostate can then be seen on a screen. This is called a transrectal ultrasound (TRUS).
-
Your healthcare provider will use the TRUS picture as a guide. They'll use a thin needle to remove tiny tissue samples from some sites in the prostate.
-
These tissue samples are sent to the pathology department. They're looked at under a microscope so a diagnosis can be made.
Risks and possible complications of core needle biopsy
-
Infection
-
Blood in urine, stool, or semen
-
Difficulty passing urine
-
Pain
-
The biopsy misses the tumor (false negative result)
Home care
You may have had the biopsy done through your rectum (transrectal), through the urethra (transurethral). or through the skin between your scrotum and anus (transperineal). Your healthcare provider will tell you what to do after the biopsy. These instructions are based on your health condition, the type of biopsy, and your provider’s practices.
-
Your provider may have you take pain medicine, such as acetaminophen for discomfort or pain. Usually nonsteroidals, such as aspirin, ibuprofen, and naproxen are not recommended because they may cause bleeding. Let your provider know all the prescription and over-the-counter medicines, supplements, vitamins, and herbs you currently take.
-
You may be asked to do only light activities for the next 24 to 48 hours after your prostate biopsy
-
You may need to take antibiotics for several days. This will help prevent an infection. Signs of an infection include chills, pain, or fever. Call your healthcare provider right away if you have any of these symptoms.
-
For the first several days drink extra amounts of fluids to help flush out the bladder, prevent infection, and reduce the amount of blood in your urine. Drinking water is best. Stay away from coffee, alcohol, and high sugar beverages as they may irritate the urinary tract
-
You may see minor bleeding after the procedure. This is normal and often needs no treatment. You may see blood in your urine or semen (rust color). Discoloration of the semen may last for several weeks. You may also have light bleeding from your rectum if you have hemorrhoids. Any lasting or increasing blood in the urine or from the rectum should be reported to your healthcare provider right away.
-
When you urinate, you may go more often, feel burning, and see pink-tinged urine after the biopsy. But since these can also be signs of a urinary tract infection, it is important to report any of these signs to your healthcare provider right away if it seems bad or lasts more than a couple of days.
-
Your provider will tell you when you can go back to your normal activities. This includes sex, exercise, and straining physically. Discuss these with your provider.
When to get medical advice
Call your healthcare provider or get medical care right away if any of these occur:
-
You aren’t able to urinate, with or without your bladder feeling full, or see that you have less flow of urine
-
Chills
-
Fever of 100.4°F (38°C) or higher, or as directed by your provider
-
Severe pain
-
Signs of an infection that's getting worse. These include pain that gets worse, pain in your side under the rib cage or in the low back, or bad-smelling urine.
-
Blood clots or bright red blood in your stool or urine
-
You feel confused or very tired
-
Your lower belly feels firm over your bladder area
Online Medical Reviewer:
Melinda Murray Ratini DO
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Shaziya Allarakha MD
Date Last Reviewed:
10/1/2024
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.