Spinal Cord Injury (SCI) and Pressure Injuries
A pressure injury is a sore caused by too much pressure on the skin. This reduces blood flow, damaging skin and underlying tissue. The result is a wound that can be quite serious. Having an SCI makes you more likely to get a pressure injury. But there are steps you can take to help prevent these sores or catch them early when they’re most treatable. Your healthcare team has likely talked with you about pressure injury prevention. Now it’s up to you to put what you learned into practice.
Why pressure injuries develop
Having an SCI affects your ability to feel and to move. It also causes skin changes that may make your skin more fragile. The conditions that lead to the development of pressure injuries include:
-
Pressure. Pressure forms anywhere your body presses into a surface. Commonly, this is a mattress or your wheelchair seat, back, or footrest.
-
Rubbing. This is also called “shearing” and “friction.” It happens when your skin slides against or across a surface. Examples are clothing or bedding, part of the bed or wheelchair, or even the underlying bone.
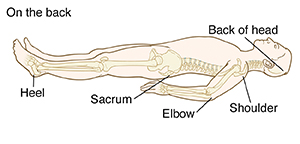
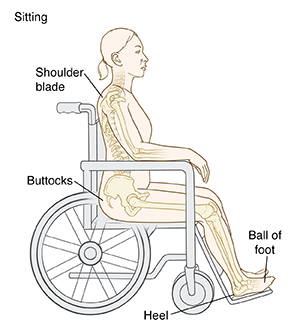
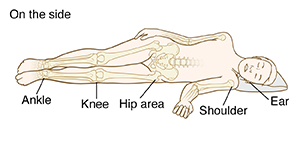
Where pressure injuries develop
Pressure injuries are most likely to form where bones are felt right under the surface of the skin. These include your:
-
Shoulder blades
-
Elbows
-
Tail bone
-
“Sit bones” (buttocks)
-
Hips
-
Ankles
-
Heels
Pressure on your skin will change depending on whether you are sitting up or lying down, and whether you lie on your back or side.
Steps to prevent pressure injuries
Your care providers will help outline the pressure injury prevention plan that’s best for you. The main steps to help keep skin healthy and prevent pressure injuries are listed below. Depending on the extent of your injury, you may need help doing some or all of these steps. Be sure to:
-
Change positions regularly. Your provider will give you guidelines for how often to shift your weight when you’re in bed or in your wheelchair. In general, change your position (or have someone help you move) at least every 2 hours while in bed or every 15 minutes if sitting. To prevent rubbing, lift your body, don’t drag it.
-
Check your skin twice a day. Look at and feel your skin carefully. Check especially over your bony prominences. Use a mirror to see behind you or where you can’t reach. If you can’t use a mirror, ask someone else to check the area. Inspect your skin once in the morning and once in the evening. Look for any of the warning signs listed in the box below.
-
Keep skin clean and dry. Clean and dry yourself after sweating or a bowel or bladder accident. Avoid harsh soaps or alcohol that dry out the skin.
-
Use the right equipment and check it regularly. Your care team can help you find the devices and equipment that are best for you. Be sure to check that things like your wheelchair back and cushion have not worn out.
-
Eat well and stay active. These will help keep your skin and body healthy, so pressure injuries are less likely to form.
When to call your healthcare provider
Check your skin daily for the following. If you notice any changes or problems, call your healthcare provider or seek medical care right away.
-
Skin redness that doesn’t go away in 15 minutes
-
Skin changes that become an open wound
-
Other skin color changes
-
A spot that is soft, warm, or cool
-
Swelling
-
Scrapes, cuts, or blisters
-
A spot that hurts or itches (if it has sensation)
Pressure injuries can start deep below the surface of the skin. So an open wound is not necessary for a pressure injury to be present.
If you see a suspicious area
If you notice an area of redness, take all pressure off that area. (This may require you to go on bed rest.) See if the skin color returns to normal within 24 hours. If it doesn't, call your healthcare provider right away. And call right away (don’t wait) if you see any open sore or other signs of skin damage.
Treatment for pressure injuries
Treatment will vary depending on your health, the size and stage of the pressure injury, and other factors. The most important thing is to keep pressure off the area. Treatment choices that may also be used include:
-
Special medical wound cleansers and dressings. Don’t use anything that isn’t prescribed.
-
Methods to remove dead tissue from the wound so it can heal
-
Antibiotics to clear up an infection
-
Medical procedures or surgery to close the wound
-
Hyperbaric chamber to increase oxygen delivery to the tissues
Monitoring a pressure injury
Pressure injuries usually start to heal within 2 to 4 weeks. While the injury is healing, watch it for signs of complications, such as infection. Inspect the injury during each dressing change. If you can’t do this, have someone who helps with your care inspect it for you. Problems to watch for include:
-
Increased swelling
-
Further changes in skin color or temperature
-
Fluids soaking through the dressing
-
Foul-smelling dressing
-
Pain (if the area has sensation)
If you notice any of these or any other problems, tell your healthcare provider right away.
Autonomic dysreflexia (AD)
Depending on the level of your injury, you may be told that you are at risk for autonomic dysreflexia (AD). This is a serious complication that needs immediate medical treatment. If AD is a risk for you, know that a pressure injury can trigger AD. If you have an AD episode, check your skin carefully for signs of a pressure injury. And if you develop a pressure injury, be alert for signs of an AD episode.
Pressure injury prevention for life
Having an SCI means having a lifelong risk for pressure injuries. So take steps every day to prevent the injuries, and check your skin for warning signs. Get help and support from your family, caregivers, and healthcare team. And if you get signs of a pressure injury, tell your healthcare provider right away. You may not be able to prevent every pressure injury. But you can prevent them from keeping you from living your life to the fullest.