When Your Child Has Tetralogy of Fallot (TOF)
Your child has been diagnosed with tetralogy of Fallot (TOF). This is a common complex heart defect. TOF is a serious heart condition, but it can be repaired with surgery.
The normal heart
The heart is divided into 4 chambers. The 2 upper chambers are called atria. The 2 lower chambers are called ventricles. The heart contains 4 valves. The valves open and close and keep blood flowing forward through the heart.
In a normal heart, oxygen-poor blood returning from the body fills the right atrium. This blood flows through the tricuspid valve into the right ventricle. The right ventricle pumps this blood through the pulmonary valve into the pulmonary artery. The pulmonary artery sends this blood to the lungs to get oxygen. Oxygen-rich blood returning from the lungs fills the left atrium. This blood flows through the mitral valve into the left ventricle. The left ventricle pumps this blood through the aortic valve into the aorta. The aorta sends this blood out into blood vessels to give oxygen to the body.
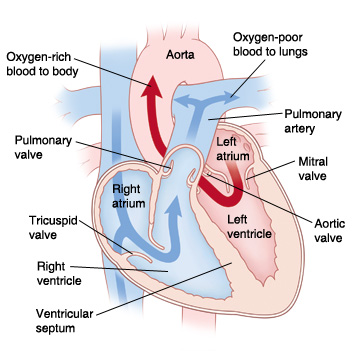 |
| In a normal heart, oxygen-poor blood is pumped to the lungs from the right ventricle. Oxygen-rich blood is pumped to the body from the left ventricle. |
What is tetralogy of Fallot?
A child with TOF has this set of structural heart problems:
-
Pulmonary stenosis (PS). The pulmonary valve or the area below or above the valve becomes narrow. This blocks (obstructs) blood flow from the heart to the lungs.
-
Ventricular septal defect (VSD). This is a hole in the dividing wall (ventricular septum) between the ventricles.
-
Overriding aorta. The aorta shifts toward the right side of the heart. This causes it to sit over or “override” the ventricles above the ventricular septal defect.
-
Right ventricular hypertrophy. The muscle of the right ventricle becomes thickened as a result of the right ventricle having to pump against the obstructed outflow to the lungs.
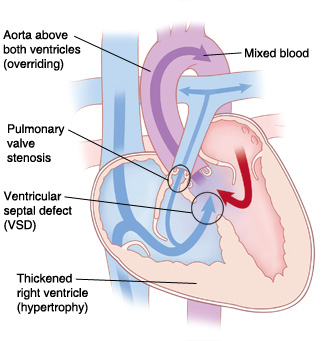 |
| With TOF, there is reduced blood flow from the heart to the lungs because the outflow of the right ventricle is obstructed. |
Why is tetralogy of Fallot a problem?
In TOF, oxygen-poor blood from the right ventricle may flow through the VSD and mix with oxygen-rich blood in the left ventricle. This is called a right-to-left shunt. The mixed blood (blood with some oxygen) is then pumped through the aorta to the body. Because this blood contains less oxygen than normal, it may cause your child’s skin, lips, and nails to appear blue. This condition is called cyanosis. Cyanosis gets worse if severe pulmonary stenosis decreases blood flow to the lungs.
A child with TOF may have sudden episodes of severe cyanosis called tetralogy spells, or “tet” spells. During these, blood flow to the lungs is suddenly and severely decreased. During a tet spell, your child may become irritable, cry, or turn blue. They may even faint or have a seizure. If your child has or previously has had one of these episodes you should get medical help right away.
What causes tetralogy of Fallot?
TOF is a congenital heart defect. This means it’s a problem with the heart’s structure that your child was born with. The exact cause of this problem is unknown. But children with certain gene problems are more likely to have TOF.
What are the symptoms of tetralogy of Fallot?
Symptoms can include:
How is tetralogy of Fallot diagnosed?
TOF may be found with fetal echocardiography (fetal ultrasound) before a child is born. This test uses sound waves to form a picture of the baby’s heart. This test can be done when the mother is at least 12 weeks' pregnant.
If TOF isn’t found before birth, signs of a heart problem may be found during a physical exam after the child is born.
If a heart problem is suspected, your child will be referred to a pediatric cardiologist. This is a doctor who diagnoses and treats heart problems in children. To confirm a diagnosis of TOF, your child may need several tests. These include:
-
Chest X-ray. X-rays are used to take a picture of the heart and lungs.
-
Electrocardiogram (ECG). This test records the electrical activity of the heart.
-
Echocardiogram (echo). This test uses sound waves to create a picture of the heart. It looks for structural defects and other problems.
-
Pulse oximeter or oxygen saturation test. This test measures the oxygen level in the blood.
How is tetralogy of Fallot treated?
A child with TOF must have heart surgery to fix the heart defects. Surgery is most often done when a child is 3 to 6 months old. In some cases, surgery may be done on a newborn baby.
In rare cases, your child may need a temporary procedure to increase blood flow to the lungs until a complete repair can be done. A surgical shunt may be needed to give stable pulmonary blood flow. Then complete repair is done when your child is older. Your child may also need a cardiac catheterization procedure. This will give the doctor more details about the condition. The doctor may also use the procedure to widen the pulmonary valve before the surgery. To widen the valve, the doctor uses a thin, flexible tube (catheter) with a balloon to stretch the valve open. Your child’s cardiologist will tell you more about this, if needed.
Risks and possible complications of TOF surgery
Risks and possible complications include:
-
Reaction to sedative or anesthesia
-
Pulmonary valve leaks blood back into the right ventricle (valve insufficiency)
-
Abnormal heart rhythm (arrhythmia)
-
Problems in the lungs
-
Infection
-
Bleeding
-
Problems with the nervous system
-
Abnormal buildup of fluid around the heart or lungs
What are the long-term concerns?
Your child will need regular follow-up visits with the cardiologist for the rest of their life. Your child likely will need more pulmonary valve treatment in the future. This may also include pulmonary valve replacement. This may be done with surgery or cardiac catheterization. This depends on the details of the surgery. Your child may also develop heart rhythm problems that may need to be treated.
After repair of TOF, most children can be active. How active will vary with each child. Check with the cardiologist about what activities are appropriate for your child.
Your child may need to take antibiotics before having any surgery or dental work for some time after TOF surgery. This is to prevent infection of the inside lining of the heart and valves. This infection is called infective endocarditis. Antibiotics should be taken as directed by the cardiologist.