RSV (Respiratory Syncytial Virus) Infection
RSV (respiratory syncytial virus) is a common cause of respiratory infections in people of all ages. RSV occurs more often in the winter and early spring. RSV is so common that almost all children have had the virus by age 2. Older adults and people who have weak immune systems can get RSV again later in life. This is because their immunity to RSV goes down over time. RSV symptoms are often mild. But RSV can be a serious problem for high-risk infants, young children, and older adults. These groups may have more serious infections and trouble breathing. Prevention choices are available for older adults, pregnant people, and newborns.
How RSV spreads
RSV spreads easily when a person with the infection coughs or sneezes. It spreads by direct contact with an infected person. For instance, kissing a child with RSV spreads the virus. And the virus can live on hard surfaces. A person can get RSV by touching something with the virus on it. These can include crib rails and doorknobs. It spreads quickly in group settings, such as daycare and schools.
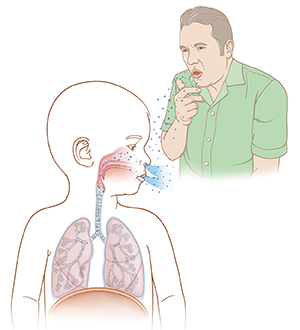 |
| Viruses that cause RSV spread through the air in droplets when someone who has RSV coughs, sneezes, laughs, or talks. |
Symptoms of RSV
Most babies and children with RSV have the same symptoms as a cold or flu. These symptoms include:
-
Stuffy or runny nose
-
Cough
-
Headache
-
Low-grade fever
Some may go on to have bronchiolitis. This condition is when the small airways in the lungs (bronchioles) become inflamed. It causes:
-
Wheezing
-
Shortness of breath
-
Fast breathing
-
Increased cough
Children, older adults, and people with a very weak immune system may get pneumonia.
Treating RSV
RSV most often goes away on its own. There is no treatment for RSV in most cases. Care for babies, children, and adults is focused on easing symptoms. Antibiotics are not used unless a bacterial infection occurs. Children or adults at high risk for severe RSV can be treated with certain medicines.
To ease symptoms:
-
Manage fever. Ask your healthcare provider or nurse about lowering you or your child's fever. Know what medicine to use. And how much and how often to use it. Never give children and teens aspirin or any medicines containing aspirin. It's linked to side effects, such as an upset stomach and intestinal bleeding. Most seriously, it is linked to a condition called Reye syndrome.
-
Dress in layers to not get overheated. Make sure your child isn't wearing too much clothing.
-
Stay hydrated. If your child is old enough, give them fluids, such as water and juice.
-
Treat a stuffy nose. For babies and young children, remove mucus from their nose with a rubber bulb suction device. Be gentle so you don't cause more swelling or mild pain. Ask your child’s healthcare provider or nurse for instructions. Consider using a cool mist humidifier to open blocked nasal passages. Older children and adults can stand in a warm shower.
-
Avoid tobacco smoke. Don’t let anyone smoke around your child. Stay out of public areas where smoking occurs.
For severe symptoms
People with severe symptoms need to be treated in the hospital. They are watched closely. They may have treatment such as:
-
IV (intravenous) fluids
-
Oxygen
-
Suctioning of mucus
-
Breathing treatments
-
Anti-inflammatory medicine, such as steroids
-
Aerosolized or oral ribavirin
-
Intravenous immune globulin
Those with very serious breathing problems have a breathing tube. The tube is put in the throat and down into the lungs. This is called intubation. The tube is attached to a machine (ventilator) that helps them breathe.
When to call the healthcare provider
Call your provider right away if you or your child have any of these symptoms:
-
Fever (see Fever and children below). For adults, call for a fever of 100.4° F (38°C) or higher, or fever that doesn't go down with medicine, or as advised by your healthcare provider.
-
A seizure with a high fever
-
A cough that's getting worse or with colored mucus or blood
-
Wheezing, breathing faster than normal, or trouble breathing
-
Flaring the nostrils or straining the chest or stomach while breathing (most commonly in young children)
-
Skin around the mouth or fingers that turns a blue color
-
Restlessness or grouchiness, can't be soothed
-
Trouble eating, drinking, or swallowing
-
Shortness of breath
-
Confusion
-
Dizziness
-
Needing to sit upright (in bed or in a chair) to breathe or catch breath
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead. This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The healthcare provider may want to confirm with a rectal temperature.
-
Ear. Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit. This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth. Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider
Preventing RSV infection
To help prevent the infection:
-
Clean your hands before and after holding or touching your child. Use an alcohol-based hand cleaner that contains at least 60% alcohol. Or wash your hands with soap and clean, running water for at least 20 seconds.
-
Clean all surfaces with disinfectant cleaners or wipes.
-
Teach your child how to wash their hands correctly and when to wash them. Have your child wash their hands often. Teach them to wash their hands for as long as it takes to sing the ABC song or the Happy Birthday song. Or have them use an alcohol-based hand cleaner that contains at least 60% alcohol.
-
Have all family members or caregivers clean their hands before and after holding or touching your child.
-
Closely watch your own health and that of family members and your child’s friends. Try to prevent contact between your child and those with a cold or fever.
-
Don’t smoke around your child. And don't let anyone else smoke around your child. This includes caregivers and family members. Don't smoke in your house or car. Keep your child out of any area where smoking occurs.
-
To prevent severe RSV in infants, CDC recommends either of these below. Most infants will not need both:
-
The antibody shot may also be advised for some infants and children ages 8 months through 19 months who are at increased risk for severe RSV.
-
Babies and children at high risk for RSV infection may get a different monoclonal antibody medicine. This is given as a series of shots (injections) once a month during RSV season. They help prevent the illness in premature babies and children with health problems, such as certain heart conditions.
-
Talk with your healthcare provider if you are age 60 or older. An RSV vaccine is available to help protect adults in this age group who are at increased risk for severe RSV. All adults age 75 and over are advised to get the RSV vaccine. Your provider can give you more information.
Date last modified: 08/15/2024